Key to understanding knee arthrofibrosis is awareness of those anatomical soft tissue areas within the joint where adhesions can form.
 First published by Dr Noyes in 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
First published by Dr Noyes in 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
Arthrofibrosis - course
- Introduction to arthrofibrosis
- The knee - range of motion
- Anatomic classification of arthrofibrosis
- What triggers arthrofibrosis?
- Early signs and symptoms of arthrofibrosis
The classification of Shelbourne (see Part 1) is important because it defines how much knee flexion and extension has been lost.
It is also useful because it identifies two major categories 'III and IV' where a very significant loss of knee motion exists.
There is a second classification system which is really the basis of all of arthrofibrosis, and that is the anatomic classification. This system identifies where the scar tissue has developed, which is what needs to be surgically addressed.
First, I will provide you with an overview of general anatomy so that we have a common starting point. Then I will discuss the anatomy as it directly relates to arthrofibrosis.

The articulating surfaces
There are two separate areas of bony articulation in the knee -
- the articulation (joint) between the femur and tibia bones (tibio-femoral joint)
- the articulation between the patella and femur bones (patello-femoral joint)
Both can be involved in the arthrofibrotic process.
The extensor mechanism
The term 'extensor mechanism' implies the unbroken chain of anatomical structures which cause the leg to extend -
- the quadriceps muscle group, stretching from the pelvis down to the tibia bone
- the tendon above the patella (quadriceps tendon)
- the patella itself within the tendon
- the tendon below the patella (patellar tendon or patellar ligament)
- the tibial tubercle where the tendon attaches to the tibia (the bony bump below the patella)
The whole of this chain can be affected by the arthrofibrosis process.
The infrapatellar fat pad
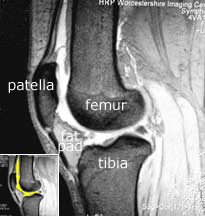
Note the relationship of the fat pad to the patellar tendon, and hence the extensor mechanism. It fills the space from the patellar tendon all of the way to the cruciate ligaments. In fact, it also extends sideways, making the bulge that one can often see in a normal knee on either side of the patella (red arrow). Normally the fat pad is not attached to either the meniscus or the patella, and is separated from the patellar tendon by the deep infrapatellar bursa.


With arthrofibrosis fat pad the fat pad becomes thickened and fibrosed, and the deep infrapatellar bursa can be obliterated. The fat pad can become adherent to the anterior horn of the meniscus and to the patella, and via the obliteration of the deep infrapatellar bursa it becomes adherent to the patellar tendon also. This thickened fat pad may also become tethered to the intercondylar notch where the cruciate lies.
Note also from the MRI that the fat pad is truly in contact with the bony lower edge of the patella. If that fat pad is scarred and contracted, can you imagine how it can pull the patella downward?
Cruciate ligaments, femoral notch and menisci
The cruciate ligaments, by their complex position of the knee, anchor the femur to the tibia. Superimpose in your mind’s eye the photograph above upon this illustration of the intercondylar notch and the cruciate ligaments. Imagine how the fat pad tucks into the femoral notch, and how easily it and the cruciates can both be involved in the arthrofibrotic scarring process.
The two menisci can also be seen in the illustration, which are located between the tibia and femur. They are held in position around their outer edges by the coronary ligaments, which attach them to the tibia.
Both the cruciate and coronary ligaments may become involved in arthrofibrosis.
Now that we have some common anatomical terminology, I will try to illustrate for you those structures which are most influential in the early progression of arthrofibrosis - the soft tissue spaces.
Flexion loss and the all-important soft tissue spaces
The soft tissue spaces become directly involved in the production of fibrous scar tissue, and this may include the following -
The suprapatellar pouch and capsular pouches
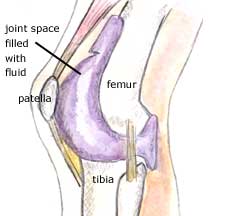
Starting from the top of the knee joint, the first soft tissue space I want to discuss is the suprapatellar pouch. This is the fold of the normal joint space which creates a pouch above the kneecap.
On the left, the inset MRI scan shows the extent of the suprapatellar pouch (yellow). In the large image, it shows up as white. Note how far this pouch extends above the patella. The fat pad is touching the patella and anterior part of the meniscus but is normally not adherent to these structures.
On the right is a three-dimensional illustration which shows the extent of the joint cavity and suprapatellar pouch when expanded with fluid.
When the suprapatellar pouch scars down, the patient will have a limitation of flexion. I want to make a few important points about this region -
- The scar tissue can be very dense and it can form underneath the muscles. The surgeon has to remove the scar tissue that is actually underneath the muscles of the quadriceps.
- In the suprapatellar pouch, a band may form which extends from the top of the patella (kneecap) to the top of the femoral condyles. It is a very dense band of scar tissue that has to be removed. This band or scar tissue may produce what we call a 'patellar clunk', where the kneecap clunks as it goes through flexion. The question is often asked if this represents actual damage to the joint. And the answer is - it may be damage to the joint, but it also may be just from the scar tissue located in that location. This same clunk may be present after total knee replacement, for the same reason.
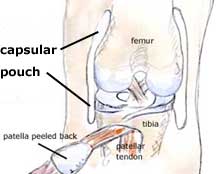
- The knee joint also has a pouch on both the medial and lateral sides. I tell my patients these pouches are like your cheeks in your mouth - like the cheeks, they have a normal extensibility or flexibility and they are usually not really very tight.
These pouches are anatomically called the 'capsular pouches' and during arthrofibrosis, they will scar down to the point of where they become adhesive to the side of the femur on both the medial and lateral aspects. Patients often complain that as they are trying to move their knee they feel tremendous stiffness - and they have - because their capsular pouches are adhesed down (adhered) to the side of the joint. The surgeon must open up those pouches to restore the normal gliding.
The patellar retinaculum
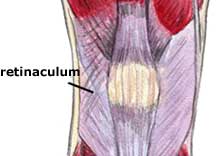
The patellar retinaculum is the fibrous tissue located on both sides of the patella -
- on the medial side, this includes the medial patello-femoral ligament that provides medial stability to the patella
- on the lateral side, the retinaculum is also part of what is termed the iliotibial band. With arthrofibrosis, this region always gets tight and patients have what we call 'limited patellar mobility'. The patient cannot glide their kneecap to the inside or the outside (which we call 'medial glide' or 'lateral glide').
Scar tissue in this region produces tremendous stiffness and blocks flexion. This scarring must be released nearly one-hundred percent of the time by the surgeon to restore a normal glide to the patellofemoral joint in a medial-lateral direction. It is very important if a patient does not have normal patellar glide, that they do not try to go past 100 degrees of flexion. This is because the tightness present in those tissues binds down the kneecap - forcing flexion may produce permanent damage to the joint.
One of the most important things that we do in our clinic is carefully stretch a knee joint, but with the recognition that in some patients, we will not be able to stretch out excessive scar tissue that is very firm and inelastic. To do so would be at the expense of the joint.
Remember, the goal of your treatment must be to preserve the joint lining (articular cartilage joint surfaces), because it is the joint lining itself that will completely deteriorate if you have a bound down knee. The medial and lateral patellar retinaculum must always be tested by the therapist and surgeon using the medial and lateral glide tests.
Quadriceps muscle and patellar tendon
The next thing that produces a loss of flexion that is very difficult to deal with is shortening of the quadriceps muscle. We documented in our studies that the quadriceps mechanism and the muscle actually shorten because scar tissue prohibits normal muscle contractions and lengthening. This muscle may start to shorten as early as four months following an injury or operation. And before that, the patellar tendon also will begin shorten, resulting in what is termed a patella infera condition.
Once the quadriceps muscle/patellar tendon mechanism goes through this shortening process, it is extremely difficult to recover the normal length. Once the surgeon has released all the tissues that I just mentioned above, the final thing that may still be limiting flexion is shortening in the quadriceps muscle and patellar tendon.
It is very difficult to measure how much shortening has occurred in the quadriceps tendon. The surgeon can get an idea if he or she can only flex the knee ninety to a hundred degrees for example. However, one can measure the amount of patellar tendon shortening using a method we published many years ago. A lateral x-ray is obtained of both knees and the height of the patella is measured, which allows interpretation of the length of the patellar tendon. The measurement of the involved knee is compared with the opposite knee, and the resulting difference indicates the amount of patella infera present.
The second factor which may limit patellar tendon medial and lateral glide is adhesion of the patellar tendon to the tibia. The normal space is lost, requiring the surgeon to free up the patellar tendon. Otherwise, it will stick down to the tibia at the top of the joint rather than its normal postion at the tibial tubercle.
Extension loss
The anatomic causes of limitation of knee extension are entirely different than those described for limitation of flexion. Four anatomical structures are of particular importance -
Posterior capsule
The first factor that limits extension is tightness of the posterior capsule located in the back of the knee. This capsule is a complex fibrous structure which encloses and supports the joint cavity. It has adequate folds in it which, in the arthrofibrosis process, get tight and are subsequently lost. This is why patients must immediately obtain zero degrees after surgery - and maintain at least this amount of extension. If extension is lost, this capsule will get very tight. This underscores the importance of immediate knee motion and flexibility programs following knee surgery.
Patients who have a chronic loss of knee extension of 10° or more and a hard, inelastic endpoint, require a posterior capsular release to regain extension and protect the joint.
Femoral notch
The next event that occurs if the knee does not reach full extension is scar tissue in-growth into the femoral notch where the cruciate ligaments are housed. This is where 'cyclops lesions' are located, and all of this scar tissue must be removed.
Hamstrings muscle
The third anatomic factor that may limit extension is the hamstrings muscles at the back of the knee. They get tight just like the quadriceps gets tight in the front. And the hamstrings can shorten - the surgeon can release everything in the knee joint, but must realize that an extrinsic cause exists (tightness and shorting of the hamstrings muscles) which blocks full knee extension.
Cruciate Ligament
Finally, in knees that have not achieved full extension for many months, the anterior cruciate ligament may actually shorten and block extension. Of course, when an anterior cruciate graft is inserted in the joint, it must be placed in the corrrect anatomic position, or the graft itself may block extension or flexion.
PREVIOUS PART: The knee - range of motion
NEXT PART: What triggers arthrofibrosis?