A total knee replacement (TKR) is a replacement of the femoral and tibial surfaces of the knee joint, and generally also part of the patella, with metal and plastic.
 Page updated February 2024 by Dr Sheila Strover (Clinical Editor)
Page updated February 2024 by Dr Sheila Strover (Clinical Editor)

X-ray of a patient's knee with a total knee replacement. Only the metal shows up on X-ray.
Indications for total knee replacement
The most common indication for total knee replacement is significant pain related to arthritis in the mature or older patient where medications and physiotherapy not longer offer effective relief.
The articulating surfaces of the joint are removed, so there is no going back after a total knee replacement.
Components of a total knee replacement
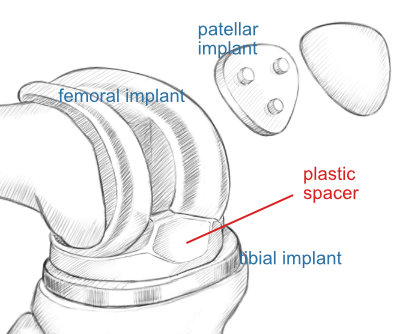
Total knee replacement usually implies replacing all three of the articulating areas in the knee with implants comprised of metal and plastic. A femoral and a tibial implant replace the two joint surfaces between femur and tibia, and a patellar implant replaces the joint surface between femur and patella.
Between the two larger implants is a plastic spacer, which effectively replaces the two menisci.
-
Quote from peer-reviewed paper:
"The perfect knee arthroplasty does not exist but the key of the success of this type of surgery depends on the correct balance between anatomical design and kinematic functionality."
Citation: Vaienti E, Scita G, Ceccarelli F, Pogliacomi F. Understanding the human knee and its relationship to total knee replacement. Acta Biomed. 2017 Jun 7;88(2S):6-16. doi: 10.23750/abm.v88i2-S.6507. PMID: 28657560; PMCID: PMC6178997.

If you look at the implant from the back, you can better appreciate that each rounded condyle of the joint is really a separate articulation (or contact point). In a partial knee replacement the surgeon can replace just one of these articulations. In fact, even in a so-called total knee replacement it is quite common for the surgeon to avoid replacing the patellar implant if the joint cartilage there is still good.
Steps of total knee replacement surgery
The surgeon will walk through the following stages during surgery:
- Shaping the end of the femur
- Shaping the top of the tibia
- Cementing the femoral component into place
- Cementing the tibial tray into place
- Attaching the plastic spacer
- Shaping the back of the patella
- Cementing the patellar button into place
- Closing the wound in layers
Watching out for complications
Rehabilitation is commonly started some time before the surgery, to optimise range of motion and muscle strength and give the patient the best chance of early mobilisation. It is critical to prevent clotting (deep vein thrombosis) and infection as a result of surgery, and blood thinners (eg heparin) and antibiotics are administered for a period before surgery. The most dreaded complication is infection which may result in months of treatment, and even temporary removal of the implant until the joint is clear of the infection.
-
Quote from peer-reviewed paper:
"....male, procedure type (bilateral, revision), [length of stay] (≥35 days), and use of transfusion were shown to be risk factors of postoperative complications following [total knee arthroplasty]."
Citation: Ko MS, Choi CH, Yoon HK, Yoo JH, Oh HC, Lee JH, Park SH. Risk factors of postoperative complications following total knee arthroplasty in Korea: A nationwide retrospective cohort study. Medicine (Baltimore). 2021 Dec 3;100(48):e28052. doi: 10.1097/MD.0000000000028052. PMID: 35049222; PMCID: PMC9191393.
Relevant content -
Special considerations -
- Total knee replacement operating room considerations
- Rehabilitation after total knee replacement
- Total knee replacement failure and revision.
 2009 - Knee Replacement - course - by Dr (Mr) Kirti Moholkar (Knee Surgeon)
2009 - Knee Replacement - course - by Dr (Mr) Kirti Moholkar (Knee Surgeon)
Other interesting material from Knee Surgeons -
- 2020 - What does metal allergy mean for patients waiting to have knee replacement surgery? - by Dr (Mr) Tarek Boutefnouchet (Knee Surgeon)
- 2006 - Heterotopic ossification after total knee arthroplasty Authors: Atamaz F et al. - interpreted by Dr Sheila Strover (Clinical Editor)
- 2017 - Non-surgery factors affecting knee replacement - by Prof Raju Vaishya (Knee Surgeon)
 2018 -
2018 -