MRI is an abbreviation for Magnetic Resonance Imaging and it is a non-invasive method of visualising the anatomy of the body.
If you have a knee problem, in most situations I believe it will be helpful for you to have such an MRI scan of your knee - to make or support a diagnosis or to exclude other reasons for your problem. MRI scans are particularly useful in the evaluation of meniscus tears, and tears of the anterior cruciate ligament (ACL) and other ligaments. If your main problem is knee pain I believe you should in most circumstances as part of the investigation have an MRI scan of the knee, and indeed I feel you should not have an arthroscopy unless you have had an MRI evaluation. The price has declined considerably over recent years, making MRI a much more affordable aid to diagnosis, and today a knee MRI is close to 400 euros in Denmark (where I practice).
How does MRI work?
MRI does not use X-rays, but relies on magnetic fields and radio waves to accentuate the interfaces between the body tissues. By creating magnetic field gradients the different tissues show up differently, and then the machine can generate images of the knee and output these digitally, allowing the physician to view the body 'in slices' and from any angle. Although every anatomy student is taught this skill of looking at a series of two dimensional slices and visualising the anatomy in three dimensions, nonetheless it requires considerable skill of interpretation when it comes to the intricate anatomy of the knee.
Both open and closed MRI scanners exist, and as far as I know the quality from the closed ones is always better. You are supposed to lie supine (on your back) and claustrophobia is seldom a problem since your head is outside the machine.
In most situations MRI is very precise; however there are a number of exceptions. I will try to explain some of those here and what you need to aware of.
Not an answer book
First of all an MRI of the knee not an answer book. A good clinical examination, in combination with your history about how the problem started and what type of pain or problem you might have, can be even more precise. Some things can not be found by either clinical examination nor by an MRI scan and you may need to undergo an arthroscopy of your knee to make a diagnosis.
What can typically be overlooked in an MRI scan of the knee?
Kneecap problems associated with anterior knee pain
I believe that one of the most common problems resulting in anterior knee pain and where the MRI findings seem to be normal is a synovial plica, since this anatomical structure can be difficult to evaluate on an MRI. Another problem - trochlear dysplasia - is also often overlooked, and the same with patella alta. The reason that these last two might be missed is that the radiologist and/or the orthopaedic surgeon do not know how precisely to make the measurements that help to diagnose these disorders. In Denmark where I work some departments have, for example, in the evaluation of these kneecap problems cancelled the axial view, in order to save time and money. Nevertheless, it is the axial view that is the most important in respect of kneecap instability and anterior knee pain, since the axial view is where the trochlear dysplasia is noticed and the lateral trochlea inclination angle, the trochlear asymmetry and the TT-TG or TT-PCL are measured. So if those measurements are not mentioned and you have kneecap problems, ask the orthopaedic surgeon about those and if he does not know how to do the measurements, perhaps you should ask for another orthopaedic surgeon...?
A high-riding kneecap - patella alta - also requires one to understand that what is important is the overlap between the patella and the trochlea - some individuals might have a very short trochlea and this means they actually have a functional patella alta, and this needs to be deliberately excluded in the MRI evaluation of this area. The radiologist should calculate the patellotrochlear index, which is more clinically relevant measurement of patellar height than older types of measurements such as the Insall-Salvati and Caton-Dechamp indexes which are obsolete and imprecise and not say anything about the articulation between the patella and trochlea, and that is what patella alta is all about. The patellotrochlear index is currently the only correct way to evaluate the height of the kneecap.
Meniscus tears (especially ramp lesions and root tears)
If a meniscus tear is suspected you can be 90% or more sure that the MRI will reveal this tear. However, in some situations you might be unlucky and suffer a tear that is localised just between sequential MRI slices and therefore not visible.
You might also have what is called a meniscus ramp lesion - that means that the meniscus is torn away from the capsule in the rear part of the knee. These tears are frequently associated with anterior cruciate ligament (ACL) injury. Meniscus ramp lesions can be difficult to see both on MRI and during arthroscopy, and as a consequence this tear is often overlooked.
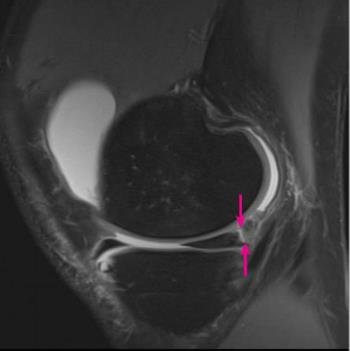
In the figure on the left you see an MRI slice of the knee from the side and the red arrows are pointing at a meniscus ramp lesion; however it is rather seldom the lesion is so clearly seen. Often a ramp tear can be overlooked because a little scar may cover the defect, and this also applies during arthroscopy, and therefore careful exploration might be necessary.

Also meniscus root tears might be overlooked on an MRI scan and reported simply and incorrectly as a radial meniscus tear. However a meniscal root tear can be very detrimental to the knee and in most cases surgery is indicated and the torn area needs to be properly dealt with. On the left you can see a meniscal root tear before and after arthroscopic repair.

The MRI scans on the right show two features of such a tear. The left MRI shows the 'gap' sign, where a white gap exists where it should be filled with the meniscus (which normally shows up as black). On the right MRI you can see that the untethered meniscus has slipped over (or extruded) over the edge of the tibial platea upon which it normally sits.
Anterior cruciate ligament (ACL) issues
In most situations an ACL tear is demonstrated very precisely on MRI. However there are exceptions. In some cases the ligament is not actually torn, but simply overstretched and has become too long to be competent. This can be difficult to see on an MRI, but a clinical examination will in most situations reveal the laxity. If you have already had an ACL reconstruction and the knee has become loose again, this can also be difficult to see on an MRI, since the ACL graft will in most situations not become torn, but just slowly gets longer and longer.
Articular cartilage problems
MRI scan can be very clear when there is a large cartilage lesion, but smaller lesions can be difficult to detect. In those situations arthroscopic evaluation gives a much more precise picture.
