Complex Regional Pain Syndrome (CRPS) - formerly known as Reflex Sympathetic Dystrophy (RSD) - was initially diagnosed over a century ago.
However, despite its unquestionable existence, it is often diagnosed late and re-injury of the same or different limb is not uncommon due the characteristics of the disease.
Much of the research has been done only within the last decade - more research is required before this complex disease is better understood. Research indicates that CRPS is a neuropathic pain disorder with autonomic features.
The pathophysiology and impact of the involvement of the sympathetic branch of our autonomic nervous system is what makes this disease relatively unique, poorly understood and multifactorial (Bruehl, 2010). It is believed that the peripheral and central nervous system are involved and deeply sensitized. Inflammatory mediators, genetics and psychophysiological components (psychologic states such as anxiety that bring about a physical response) are also involved in addition to the inexplicable contribution of one's altered sympathetic nervous system pathways.
In regards to genetics, those siblings of patients diagnosed with CRPS were statistically more likely to suffer the diagnosis (Kirkpatrick, 2003). Additionally those who had complications of CRPS after a surgery or injury were far more likely to sustain CRPS should they undergo surgery on an unrelated body part. This is important to note as clinicians, in particular surgeons, rarely warn patients of this increased risk, prior to surgery. A CRPS patient may was the pros and cons quite differently than a person without increased risk.
CRPS Symptoms
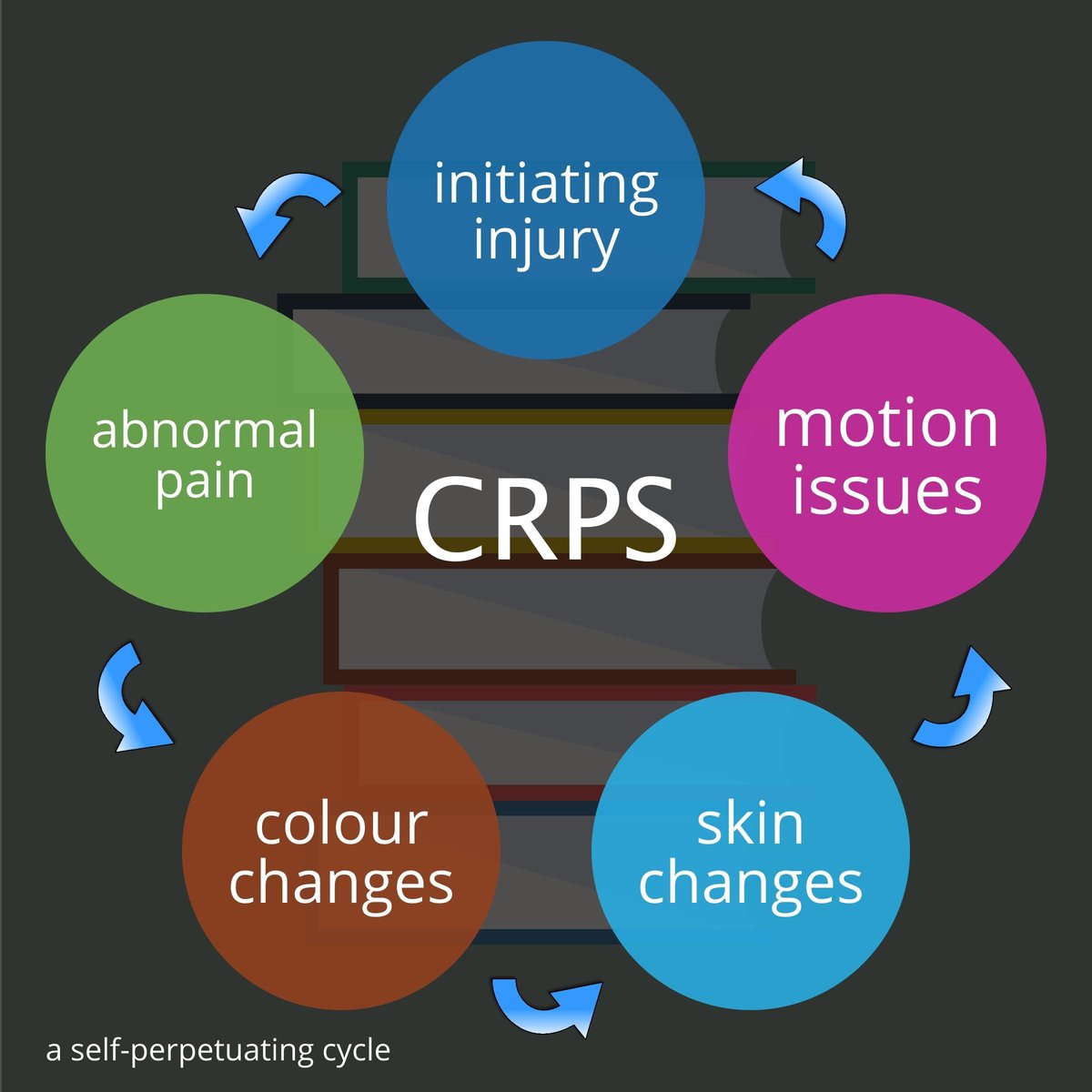 There are six global clinical symptoms that constitute the diagnosis and when delineated it is easy to see why they make a patient prone to re-injury:
There are six global clinical symptoms that constitute the diagnosis and when delineated it is easy to see why they make a patient prone to re-injury:
- PAIN - The hallmark feature of the disorder. The pain may be described as stabbing, burning, deep or aching. They may experience pain from a stimulus as normal as clothing touching the extremity (allodynia). This pain may cause difficulty with ambulation and make one more prone to falls due to atrophy of muscles and the inherent weakness this may cause. Also, a neuropathic pain may cause difficulty in position sense (proprioception), affecting balance and coordination of walking. This can also lead to falls.
- SKIN CHANGES - The skin may appear shiny over the affected limb (dystrophy); alternately, it may become scaly in appearance. Normal hair growth may be altered with hair coming in more sparsely or become coarse in texture. The skin color may also change, for example becoming spontaneously pale. These changes are rarely constant but transient (taking a quick photo with your phone may assist your physician to detail the objective findings of this condition as pain - the hallmark - is subjective). The skin may experience “goosebumps” with piloerection of the affected limb. Nail growth may be affected. A faster nail growth is often seen with CRPS.
- SWELLING - The affected limb will also oftentimes remain swollen. Sometimes this chronic swelling will change the skin texture into a brawny edema. This swelling can also cause proprioceptive disturbance and falls may occur secondary to this. Swelling with a demarcation line is almost diagnostic of CRPS.
- MOVEMENT DISORDERS - Patients almost universally complain of joint stiffness. This stiffness may also place one at risk for falls. Muscle wasting (atrophy) is also a secondary complication of this lack of movement. One diagnostic finding is after a sympathetic nerve block that the stiffness improves substantially for a period of weeks after the block is given. This is lends further credence to the diagnosis of CRPS (Kirkpatrick, 2003). For some patients stiffness and abnormal muscle tone (dystonia) prevail, but dystonia is at the severe end of the spectrum and some clinicians may perceive this as a psychiatric symptom, further delaying diagnosis. The patient may also be “branded” by a less well-trained clinician with a psychiatric diagnosis that follows them for a lifetime.
- BONE CHANGES - Patients may get a 'patchy' osteoporosis, so that they are more prone to a fracture with little trauma. This patchy osteoporosis can be seen on radiographs or with a bone scan.
- VARIABLE DURATION - The duration is highly variable. Mild cases may last only a few weeks and remit. In most cases symptoms last for years. Some patients have symptoms indefinitely. Additionally, periods of remission and exacerbations are not unheard of.
- SPREADING SYMPTOMS - Patients with CRPS often will have a spread of the symptoms to an additional part of the body. There may or may not have been a new injury - cases vary. Certainly, if one has had CRPS in a hand, for example, they are much more likely to acquire CRPS in an additional limb when injured.
Citations:
Veach RM, Montgomery AA, Dahlberg K. Complex Regional Pain Syndrome: Reasons Physicians do not follow Clinical Guidelines. Journal of the American Medical Association, 2000; 283: 1685-1686
Bruehl, S. An Update on the Pathophysiology of Complex Regional Pain Syndrome. Anesthesiology 2010 Sep; 113 (3) 713-725
Kirkpatrick, Anthony MD, PhD RSD/CRPS International Update on CRPS: Clinical Practice Guidelines, third edition. Symposium 2003 www.rsdfoundation.org
