After taking the history from the patient, a surgeon is trained to follow a routine of examination, so that signs are not missed.
Because we are working within a narrow framework for this course, I am only going to discuss those elements of the examination pertinent to the topic of pain around the kneecap.
The history will by now have offered many clues as to the nature of the problem. Examination by the clinician will help to confirm or refute each of the diagnoses which the clinician is contemplating.
Examination standing
The patient must first be examined in the standing position.
- long bone rotation - With the feet pointing forward, are the patellae pointing straight ahead? If they are pointing inwards ('squinting patella') or if they are pointing outwards ('grasshopper knee caps') they indicate a serious underlying variation in limb alignment commonly referred to as miserable malalignment.
- ligament laxity - Does the patient stand in a back-knee'd position? As the patient walks, is he or she flat-footed? This reflects loose ligaments.
- feet - Look at the heels from behind. Do the ankles seems to roll inwards?
Sitting at the edge of the examination table
The patient sits with the legs hanging over the side of the examination table. From this position one can assess -
- high patella - With the patient sitting at the edge of the examination table, one may note a high-riding kneecap (patella alta). Indeed, in severe cases the patella does not point straight ahead, but is directed towards the ceiling.
- abnormal groove - The patient is asked to straighten the knee. The kneecap should be moving up and down in a straight line. If, as the knee nears extension, the patella lurches to the side, the patient is said to exhibit a J sign. This is an indication of considerable bony and/or soft tissue abnormality at the top of the trochlear groove.
- cartilage damage - As the patient actively flexes and extends the knee, the examiner's palm is placed against the patella. Pain and/or grinding can be elicited, suggesting the presence of cartilage changes under the kneecap. This is a widely accepted test though to my knowledge it has not been tested for accuracy. A light crunching sound called 'crepitus' is sometimes heard as the patient bends and straightens the knee. There is no universal agreement on the significance of this finding.
Supine (lying on one's back)
In this position the clinician can examine -

[All illustrations on this page are reprinted with permission, The Adult Knee, Chapters 59-60, Lippincott Williams & Wilkins, 2003.]
It is present in only the most severe forms of instability and, as such, is not a good screening test for patellar malalignment or even instability. However, when it is positive it usually indicates a serious anatomic variation or injury that will probably require surgery.

- patellar tilt - The normal kneecap lies flat. In other words, an imaginary line drawn between the borders of your kneecap should be parallel to the floor. In some patients the kneecap is tilted instead, like a beret. This is a form of so-called malalignment. A subset of such patients will have pain as a result of this malposition.
- tenderness under the patella - Patients with painful malalignment commonly exhibit tenderness about the patella. If the patella is tilted but not tender, the doctor should look elsewhere for a source of pain - it's not the patella.
- q-angle - At this point, the 'quadriceps' (Q) angle can be assessed. This somewhat complex angle starts way up at the hip and goes just past the knee. It reflects the relationship of various muscles and tendons about the kneecap and is one measure of how likely the kneecap is to be pushed off to the side. The normal is 15-20 degrees. When the Q angle is elevated (20 degrees or more) this represents another form of malalignment.
A common error among health professionals is to assume that the Q angle is the angle between the femur and tibia.
Although it is GENERALLY true that higher fem-tib. angles lead to higher Q angles and that lower fem-tib. angles lead to lower Q angles, it is not always true -which is why the lower limb of the Q angle is the a funny line from the center of the patella to the tibial tubercle, and not simply the axis of the tibia.
There exist a number of patients with tibia vara - the exact opposite of a knock-knee - and a large Q angle. This is because their tibial tubercle is quite lateralized.
I usually state that normal is 15-20 degrees, mainly because these are round numbers. I don't think you can be accurate within a degree with standard measuring tools.
High Q angles are bad, but low angles lead to fem-tib. arthritis [the downside to medializing the tibial tubercle on everyone], so we can't say that the lower the better. There's a healthy range.
Prone (lying on one's stomach)
In this position one can assess -
- hips - With the patient prone (on his/her stomach), the doctor measures the range of motion of the hips, since hip abnormalities can contribute to knee pain.
- hollow of knee - The popliteal space (back of the knee) is evaluated for the presence of masses such as a Baker's cyst (a simple reservoir of fluid).
Decubitus position (lying on one's side)
In the decubitus (side) position the patient is evaluated for tightness of the iliotibial band (ITB) by way of the Ober test. Ober's test is the test for tightness of the ITB.
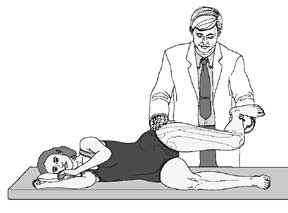
The subject is placed on their side, healthy side down. The knee is flexed 90 degrees and the hip extended to neutral (no flexion).
The doctor holds the leg up by the foot. Normally, the knee falls down to the exam table. If the ITB is very tight, the leg hangs up in the air (very impressive). If it's moderately tight, the knee falls halfway to the table.
This is also a useful position for examination of the hip.
In my experience, the Ober test is more likely to be present in patients with patellar pain than in patients with instability. It is one of the most commonly overlooked tests in orthopedics! And yet a tight ITB will not be detected by any imaging study! Like the neuroma, if the diagnosis is not made on the physical examination it will be missed entirely!
Part 5 was only a brief overview of the history and examination. What I am hoping you have noticed is that it is not possible to assess the knee without a proper history. Nor is a cursory look at the knee the sign of a competent doctor.
If nothing else, I hope at least you take away with you an overview of what you should be expecting from your doctor!
PREVIOUS PART: Symptoms associated with patellofemoral pain
NEXT PART: Imaging and X-rays for patellofemoral pain
 Page first published 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
Page first published 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
Dr Ronald Grelsamer has decades of experience in managing problems of the knee related to the patella. In this course he gives a comprehensive overview of those conditions that can cause pain in the patellar region.
