Dr Stone presents a patient with an osteochondral defect treated with paste grafting.
 First published 2010 by Dr Kevin R Stone, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
First published 2010 by Dr Kevin R Stone, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
- Video - The paste graft technique
- Video - Meniscus cartilage replacement for arthritis
- Video - Lateral meniscus allograft transplantation
- Videos - Knee Dislocation: ACL Reconstruction - PCL Reconstruction / Reconstruction of posterolateral corner
- Treatment of failed Osteochondritis Dissecans repair by Articular Cartilage Paste Grafting
- Combined Meniscus Allograft Transplantation and Articular Cartilage Paste Grafting
- Collagen Meniscus Implant
A 42-year-old female initially injured her knee skiing as a child at age 10.
She underwent surgical treatment of the knee with removal of a portion of the medial meniscus and was casted for a week at that time. Her treatment then left her with an injured knee that did not permit her to return to sports or normal activities of youth. She recalled when we first met her that she had had pain for many years. She reinjured her knee at age 39 rollerblading. She underwent arthroscopy three months later for partial medial meniscectomy and removal of a loose osteochondral fragment. One week after surgery, she reinjured herself turning over in bed and withstood the pain for a year and a half before clinical evaluation.
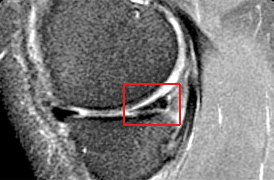
She presented to us with the MRI seen below. The red box on the MRI is over the medial meniscus cartilage. The MRI documents a chronic meniscus degenerative tear which had failed to respond to a partial meniscectomy. The options at this time when she presented to us were to repeat the meniscectomy. However, given the fact that it had already failed this did not seem to be a likely successful course of action. Therefore we planned to do a meniscus reconstruction where we would use a collagen scaffold as a regeneration template to regrow the missing meniscal tissue and therefore provide the shock absorber that her knee so clearly needed.
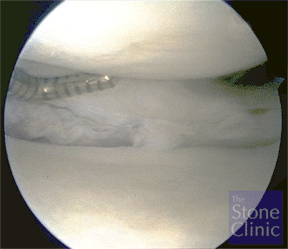
At the time of arthroscopy the meniscus was found to be chronically torn and degenerative as seen on the next picture. A meniscectomy if it had been performed at this time would leave her with essentially no meniscal rim and no protection for the joint – therefore a collagen meniscus implant was prepared as you can see in the photo on the right with a suture placed through the meniscus in order to help pull it into the knee after it was sized for the defect.
At presentation
The patient presented with moderate pain, slight swelling, and difficulty ascending and descending stairs. She had pain with palpation of the medial joint line, and positive Apley’s and McMurray’s tests of the medial meniscus.

MRI (on right - a side view) revealed a tear of the posterior horn of the medial meniscus with inferior surface extension. MRI's are digital 'slices' through the body - this slice is from the side through the area of the meniscus at the back o the knee - the triangular bit in te red box is a cross section of the meniscus there - you can see that there is an interruption of the density of the structure.
The patient underwent surgery - which was two years after the most recent injury - for medial meniscus reconstruction using a collagen meniscus implant.

Surgery revealed a large complex, degenerative tear of the medial meniscus. The undersurface of the meniscus appeared to be sheared off and displaced into the joint. The tissue was debrided back to a stable base. The defect size was measured with a calibrated probe and noted to be 24 mm in length and 6 mm in length. The collagen meniscus implant (photo on right) was trimmed to match. The implant was soaked in venous blood for one minute and then inserted into the meniscus defect. Stitches were placed to secure the implant to the native meniscus tissue.
The follow-up MRI at three weeks demonstrated excellent position of the collagen meniscus implant. You can see also that the density of the meniscus is more uniform now.
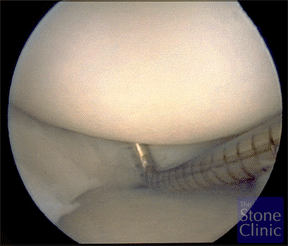
A follow-up second look arthroscopy with biopsy was perfomed three months later per the IRB approved FDA protocol. The implant was in place with new healed, regenerated tissue. A 2 mm defect in the radial plane was noted. The picture on the left shows an arthroscopic probe probing the regenerated meniscus tissue.
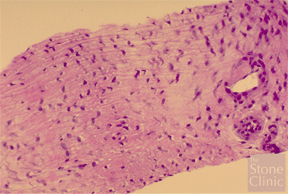
The biopsy was obtained from the superior to inferior surface. The photo of the biopsy on the right demonstrates the cellular migration of the meniscal fibrochondrocytes (cartilage cells of the kind that produce fibrocartilage rather than pure hyaline cartilage) into the collagen meniscus implant, demonstrating that it worked effectively as a regeneration template.
Five-yearly follow-up
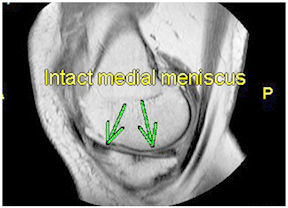
The patient was seen annually for 5 years then every five years thereafter with a full return to sports without pain. The patient returned for her 15-year follow up evaluation and reported no pain. MRI documented an intact medial meniscus, with a subchondral osteophyte within the medial femoral condyle and a small ganglion cyst medial to the MCL.
Discussion
The decision to do a collagen meniscus implant versus meniscectomy was based on the logic that meniscectomy alone had already left her with a painful knee. The arthroscopic photographs demonstrate a significant meniscal defect. However the remaining portion of the meniscus cartilage was intact and therefore there was no indication to do a complete meniscus replacement using an allograft. Given the fact that the patient was only 39 years old and had a relatively healthy articular cartilage throughout the joint, joint arthroplasty would not be indicated.
Patient's perspective
PREVIOUS PART: Combined Meniscus Allograft Transplantation and Articular Cartilage Paste Grafting
END OF COURSE.
