Tissue engineering will greatly expand our ability to restore damaged knees, and other joints: and research in these areas shows great promise.
For now, however, this case exhibits the cutting edge of knee restoration technology as it exists today and illustrates how far we have advanced even in the last few years. Indeed the chief purpose in writing this article is to disseminate information as to what is available in this fast moving field in which we can now restore more than most patients, and even physicians, currently realize.
All traumatic or degenerative joint problems relate to one or more of the above and we now have at least one restorative procedure for each of these components of knee health if it is affected, as follows -
Patients in need of restorative surgery typically have one procedure, usually as an outpatient, and sometimes two. ACL/HTO, MF/HTO, and ACI/MAT are frequently performed combinations. These procedures have high efficacy rates. For example, we recently reported a 100% success rate in restoring knee stability in the largest hamstring ACL reconstruction series in the world's literature. All are FDA approved and all are paid for by health insurance. However, we are now able to address even more complicated cases that formerly would likely have required knee replacement.
Presented below is one such case -
ACL RECONSTRUCTION: In July of 1996 she twisted the same knee and felt it go out of place and came to my office. She was 35 years old at that time, 5foot 8inches tall and 180 pounds. The KT 1000 test after that injury showed her normal knee to have 4mm of laxity and the injured left knee to have 10mm, diagnostic of Anterior Cruciate Ligament (ACL) tear. Her knee felt unstable with activity. On August 28 th 1996 I reconstructed her left knee, as an outpatient, using a part of her hamstring tendon to make a new anterior cruciate ligament. Her lateral compartment was normal. Her medial meniscus was absent. The articular cartilage in the medial compartment was thinned but at that time had no full thickness defects down to bone. She had excellent restoration of strength,'normal' stability as measured by the KT 1000, and was pain free with he regular activities after the ACL reconstruction.
MENISCAL DEFICIENCY ARTHRITIS: After her rehab was complete she was not seen again until 2002. At that time she described that while she had no instability she now had developed constant aching pain that greatly interfered with her life. This was a result of the removal of the medial meniscus from her knee some 30 years previously that resulted in a slow premature arthritic degeneration. X-rays and MRI showed a loss of 50% of the cartilaginous joint space of her left knee where her medial meniscus had been removed and also now showed full thickness defects in her articular cartilage.
ARTHROSCOPIC MICROFRACTURE: We elected to treat her articular cartilage with an arthroscopic microfracture (MF) to see if this would be sufficient without having to perform more invasive open surgery. On June 28 th 2002 she underwent a microfracture (MF) in which full thickness articular cartilage defects in her medial femoral condyle and medial tibial plateau were treated. She was pain free for about one year; however in May of 2003 her pain returned. We decided to take the next step and replace her meniscus with a cadaver allograft meniscus (MAT). We also decided to take a specimen or biopsy of her own cartilage cells at that time for later implantation (ACI).
LEG ALIGNMENT: Her leg alignment was then evaluated using special hip-knee-ankle mechanical axis x-rays taken in our office which showed a 6 degree mechanical axis varus (bowlegged) deformity. This malalignment put extra pressure on her painful medial knee and accelerated damage to that area. In such cases the cartilage replacement procedures have a much lower success rate unless the malalignment is also corrected. Conversely, the simple act of unloading the medial compartment in and of itself results in some new regeneration of cartilage.
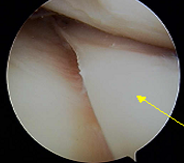
HIGH TIBIAL OSTEOTOMY: We therefore elected to proceed first with High Tibial Osteotomy (HTO) September 24 th, 2003 before proceeding with the cartilage replacement procedures. At that time I saw through the arthroscope that the microfracture had been successful in filling in part but not all of her previous articular cartilage defect necessitating the taking of the tiny specimen of some of her articular cartilage cells for later ACI. These were flown to Genzyme Biosurgery in Cambridge Mass (LINK) that same evening. The HTO corrected her alignment perfectly, from 6 degrees of varus, to 1 degree of valgus exactly as desired. During her convalescence she was in a car accident in which air bags deployed but neither herself nor her knee was injured.
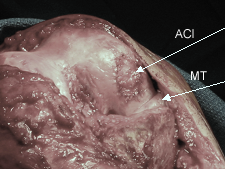
MENISCAL ALLOGRAFT TRANSPLANTATION AND AUTOLOGOUS CHONDROCYTE IMPLANTATION: In December of 2003 we proceeded with simultaneous MAT to replace the meniscus removed 30 years earlier, as well as ACI to restore her articular cartilage. The ACI uses her own cells and the meniscal allograft is repopulated by her own cells which replace the donor cells and thus also becomes a living part of her anatomy. By January she was essentially pain free and began light work at her warehouse supply store. By March she was working full time on her feet. Although she was pain free and could fully straighten her knee she could only flex it to 70 degrees despite several months of physical therapy and was no longer making progress in her range of motion. Therefore in April of 2004 she underwent arthroscopic removal of scar tissue from her knee. The allograft overall looked excellent as did the ACI graft and the prior microfracture as well as the ACL graft. Her motion improved gradually and by June she had a very satisfactory 122 degrees of knee flexion while maintaining her full extension.
When last seen in December of 2004 she had no pain, she was exercising regularly on an elliptical trainer and was fully functional. Her x-rays showed good preservation of her medial cartilaginous joint space.
Suzanne's only realistic alternative to joint preservation surgery in 2002 would have been a metal and plastic knee replacement, partial or complete, for her severe constant knee pain. Now almost 3 years later she is pain free and fully functional.
How long will she stay that way? In a severe, complex, and unique case such as hers it is difficult to say. However in the more typical simpler cases for which we have better data, the long term success rates have been excellent. And since knee replacements do not always relieve pain, wear out more quickly in younger patients, can often not be satisfactorily salvaged when they do wear out, and result in significant activity limitations even when they work well, they are always an undesirable alternative for younger (under 60) patients such as Suzanne.
Knee replacements also 'burn bridges' because the surgeon must remove large amounts of bone to fit the artificial knee in. Thus, it is impossible to do any sort of restorative procedure once the TKA (total knee replacement) is implanted: one can only do progressively more radical knee replacements if there is a problem. In contrast, if a knee restoration procedure is unsuccessful it can always be salvaged by a knee replacement procedure. As you can see, fully restoring Suzanne's knee was not easy and was even more difficult for her since she came in from out of state for treatment. However she worked hard to rehabilitate her restored knee and the results have been gratifying.
We are optimistic that Suzanne will have long term success. However even if it is shorter term it will still significantly push back the time at which a knee replacement will be necessary which will be of substantial benefit to her in several ways. First, the older a person is when they need an artificial knee the longer it is likely to last since activity levels and wear on the prosthesis decline with age. Second, technology keeps improving. For example, we now know Suzanne would need only a partial knee replacement, whereas in 2002 this technology was not as accepted and she would likely have had the more radical total knee replacement. Third, the HTO, by correcting her malalignment, renders the cartilage repair procedures and any joint replacement procedure overall more successful because one compartment of her knee is no longer overloaded with pressure. Fourth the MAT and ACI repair her knee with living tissues populated by her own cells. They are capable or healing and regenerating themselves which metal and plastic obviously are not. Fifth she does not need activity restrictions to the extent that she would with an artificial knee which wears out more quickly the more it is used. Thus Suzanne can be more active.
Age, however, is a limiting factor for 2 reasons. First the rehabilitative process can be hard on older patients for these complex procedures. Secondly, while knee replacement is a bad alternative for younger patients, it is a good alternative for older patients in whom they last longer and are less likely to need re-replacement later which has a high complication rate and much lower success rate than primary total knee replacement. Third, an older knee is less likely to be able to generate new tissue as well as a young knee. Thus, we usually cannot treat patients above 55 years of age with ACI or MAT. ACLR and HTO with MF can be used up to about age 59, and MF alone can be used in patients in their 60's and 70's in appropriate cases. For patients over 55 to 60 years of age unicompartmental (partial) knee replacement is a useful conservative option to total knee arthroplasty. This involves only an overnight hospital stay, much less bone removal, and better function than a total knee replacement. Patients over 65 years of age are usually good candidates for total joint replacement.