The tibia bone is one of the three bones making up the knee joint (the others being the femur and the patella).
The upper surface of the tibia is flattened, and this flat surface is known as the 'tibial plateau'.
The tibial plateau
The tibial plateau is covered with the shiny white joint cartilage that is critical for the smooth movement of the joint, and upon this joint cartilage are housed the two important shock absorbers of the knee, the menisci, which are attached to the tibia and to the outer capsule by short ligaments. The menisci are shaped to accommodate on their underside the flat tibial plateau and on their upper side the rounded ends of the femur bone, offering stability to this rather complex kind of hinge.
The tibial plateau is also host to the cruciate ligaments in the middle of the joint. They span from the tibial spines in the middle of the tibial plateau up into the roof of the notch between the two rounded ends of the femur bone above. These ligaments are extremely important stabilisers of the knee joint.
At the sides of the joint are another important set of ligaments reaching between the same two long bones, and these are the collateral ligaments (medial and lateral).
All of these structures may be affected by fractures (breaks) of the tibial plateau.
Type of injury causing tibial plateau fracture
The mechanism of injury is a vertical impact associated with a sideways force, and the tibial plateau may have a portion cracked away from the main bone, and the affected bit may even be shattered and depressed downwards. The majority of the fractures affect the less robust lateral part of the plateau, and in a significant number of people there is also damage to a meniscus or ligament.
Why are fractures of the tibial plateau so important?
Unfortunately these fractures are often missed, particularly the depressed fracture in older osteoporotic ladies, where the bone does not show up so well on X-rays and the depressed fracture may not be immediately evident.
Sometimes the shattered plateau is difficult to manage, and it needs a competent trauma surgeon to be able to get all the fragments back into the right position and adequately fixed.
If the meniscus and the ligaments are also damaged, the surgeon needs to make decisions about these as well, and needs to have the surgical competence to deal with meniscal tears and avulsions and to reconstruct the ligaments. There may need to be more than one surgical procedure to offer each component the best chance to heal, and usually the surgeon will wait until the fracture has united before attempting to reconstruct the important cruciate ligaments.
Classification of tibial plateau fractures
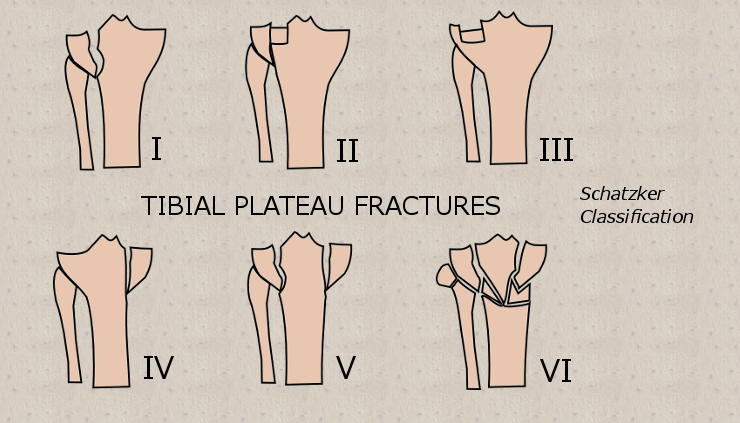
There are a number of different classification systems of tibial plateau fractures, used to record the severity of the bony injury. One of the most common is that of Schatzker1, where the degree of severity of the breaks is mirrored by the number given in the classification, with Type VI being the most serious.
Medial or lateral?
Complications of tibial plateau fracture
Early
Besides the complications above, another serious problem can accompany bad tibial plateau fractures in the early period, and that goes by the name of 'compartment syndrome'. This is when there is sudden bleeding into the tight tissue planes of the lower limb sufficient to obstruct venous return, and the increasing pressure inside the muscle compartments can lead to death of muscle tissue. Compartment syndrome is excruciatingly painful, and is usually managed by slitting open as a surgical emergency these taut areas by a technique known as 'fasciotomy'.
Because the knee needs to be immobilised while the fracture heals, knee stiffness is very likely to complicate recovery, and physiotherapy needs to be competent and proactive.
Late
Post traumatic arthritis complicates very many of the more serious of the tibial plateau fractures, even those that have had very good initial surgical outcomes.
References
1. Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968--1975. Clin Orthop Relat Res. Jan-Feb 1979;(138):94-104.
Further reading
Pearls and pitfalls in the treatment of tibial plateau fractures - http://www.aaos.org/news/bulletin/sep07/managing3.asp