Dr Hambly clarifies the difference between articular cartilage and meniscus cartilage.
 First published in 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
First published in 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
Introduction to articular cartilage repair
Mention knee cartilage to most people and they will tend to think about the wedge shaped shockabsorbers of the knee - the menisci.
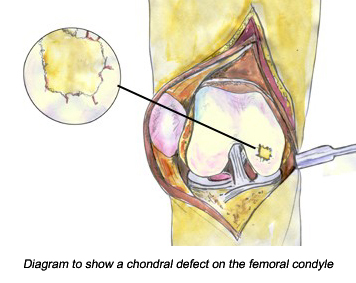
However, there is another form of cartilage in the knee that causes knee problems - the articular cartilage - the white gristle covering the adjacent surfaces of 'articulations' or 'joints'.
Articular cartilage has been known to be a potential problem for quite a while! In Roman times after gladiators had 'dissected' each other fighting, their physician, Galen, witnessed human tendons, cartilage and ligaments and made the observation that 'athletes get arthritis'. Two hundred and fifty years ago a famous anatomist noted that 'ulcerated cartilage is a troublesome thing and once destroyed, is not repaired' (Hunter 1743). Thousands of people each year experience symptoms related to chondral (joint cartilage) and osteochondral (joint cartilage and bone) defects.
We are in the 21st century now so why does articular cartilage damage continue to be such a 'troublesome thing'? Well to give you a better insight into why that is the case it is useful for you to know a bit more about the structure of articular cartilage, the role that it performs and how it gets damaged.
What is articular cartilage?
Articular cartilage is found in all moving joints in the body (synovial joints) and its role is to protect the bones by keeping the surfaces of the bones apart from each other, to absorb shock and to help make movement smooth. Articular cartilage does this by providing a protective, wear resistant surface to the end of the moving bones. In the knee articular cartilage covers the ends of the femur (medial femoral condyle, lateral femoral condyle and the trochlea), the top of the tibia (tibial plateau) and the back of the patella.

This image of the rounded end of the femur bone show the white shiny articular cartilage.

This second image shows a close up of the area circled in red.
Articular cartilage is a particular type of cartilage called hyaline cartilage (derived from the Greek word hyalos, meaning glass). Hyaline cartilage is a hard, white shiny material with a unique structure that creates a surface that allows the bones to glide easily past each other as the knee joint moves. It varies between individuals but it is generally between 2 and 4mm in depth in the knee and it has an amazingly low coefficient of friction - just 1/15th that of ice - now that's very slippery. The special nature of this material, however, also makes it particularly vulnerable once it becomes damaged.
How can you damage articular cartilage?
Articular cartilage injuries are common. The normal structure and function of articular cartilage can be upset relatively easily and damage to the articular cartilage often results. There are several ways in which your articular cartilage can become damaged.
- A sudden direct blow to the cartilage (traumatic) e.g. a high-energy injury such as a bad fall on directly onto your knee or during sporting activities.
- Slow damage to the cartilage following a knee injury (post-traumatic).
- Wear and tear over time (degenerative joint disease or DJD) - especially when there is malalignment or instability in the joint and/or if you are overweight.
- Immobilisation for long periods of time as articular cartilage is nourished by joint movement so immobilisation can result in damage.
- Osteochondritis dissecans is a condition that is thought to occur due to poor blood supply to the underlying bone resulting in a piece of cartilage and subchondral bone separating from the articular surface.
It is possible to just damage the articular cartilage on its own but you often find articular cartilage damage in conjunction with injury to other tissues in the knee particularly ligaments and menisci. If you have had a previous injury to your ligaments and/or menisci then you are at greater risk of articular cartilage damage due to the altered mechanics of the joint even if the original injury has been successfully repaired eg anterior cruciate ligament reconstruction.
A general misconception is that articular cartilage damage and osteoarthritis only affect people in their 50's or older. Although there is a greater incidence of articular cartilage problems in this age group young people damage their articular cartilage too, especially in sports or via osteochondritis dissecans.
If the knee joint is out of position (mal-aligned), unstable or if the knee cap is being pulled to one side too much stress could be placed on particular parts of the joint surface and this is known to accelerate degenerative changes in the articular cartilage. This has important implications for cartilage repair surgery that will be discussed later.
Journal publications
Additional Information
Web articles
Bobic, V. ISAKOS Current Concepts. The utilisation of osteochondral autografts in the treatment of articular cartilage lesions.
http://www.isakos.com/innovations/oats.aspx
Diduch, D.R. & Cohen, S.B. Joint repair: Treatment options for articular cartilage injury.
http://www.orthopedictechreview.com/issues/novdec02/pg24.htm
Johnson, D. Articular cartilage update
http://www.medscape.com/viewarticle/451348
Luscombe, K. & Oliva, F. A Short Basic Sciences Review of Articular Cartilage.
http://www.isakos.com/innovations/luscombe.html
Niall, D.M.& Bobic, V. ISAKOS Current Concepts. Bone Bruising and Bone Marrow Edema Syndromes: Incidental Radiological Findings or Harbingers of Future Joint Degeneration?
http://www.isakos.com/innovations/niall.aspx
Minas, T. Autologous chondrocyte implantation for chondral defects of the knee.
www.orthojournalhms.org/volume2/html/articles6.htm
Wroble, R.R. Articular Cartilage Injury and Autologous Chondrocyte Implantation Which Patients Might Benefit?
http://www.physsportsmed.com/issues/2000/11_00/wroble.htm
Tissue Engineering Companies
Ars Arthro - Patient Information
http://www.arsarthro.com/en/patient_schritt.php
Fidia Advanced Biopolymers
http://www.fidiapharma.it/files/index.cfm?id_rst=130
Geistlich Biomaterials - Patient information
http://www.geistlich.com/biomaterials/en/patients/index.html?frames/content.html
Genzyme Biosurgery - Carticel Patient Information
http://www.genzymebiosurgery.com/prod/cartilage/gzbx_p_pt_cartilage.asp
OBI OsteoBiologics - Patient Information
http://www.obi.com/patients_brochure.htm
Tigenix - Patient Website
http://www.tigenix.com/home.asp?map=h_chondro
Other Useful Sites
The Cartilage Research Foundation
http://www.cartilagefoundation.org/
Webcast of Carticel Articular Cartilage Repair
NB This webcast is not for the faint hearted as it shows video of the actual surgical procedure.
http://www.slp3d2.com/sfi_1012/broadcast.html
Cartilage Restoration Symposium Videos
NB These videos are not for the faint hearted as they show images of actual surgical procedures.
http://www.slp3d2.com/gen_1061/
