When patients struggle to regain extension after ACL reconstruction, one of the important things to exclude is the 'cyclops' lesion.
If the physiotherapist pushes the patient too hard in the presence of a cyclops, it may trigger breakdown of the articular cartilage.
The Mythical Cyclops
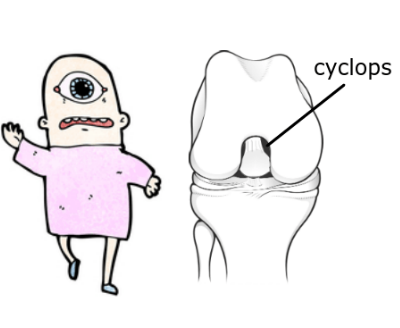
The mythical ‘Cyclops’ creature had an eye in the centre of its forehead. The ‘cyclops’ lesion that we refer to in the knee is a fibrous nodule, resembling an eyeball, localised to the middle of the rounded part of the femur, and obscuring the notch area and cruciate ligaments.
It forms in relation to damage to the anterior cruciate ligament itself, and acts to hinder extension as an actual mechanical obstruction. Although the lesions (a lesion means an ‘abnormality’) are almost always often found in this anterior location, they have been located laterally after a lateral meniscectomy procedure, but in this instance they do not interfere with extension.
Comparing a cyclops lesion to arthrofibrosis
When loss of extension does occur after ACL repair despite “aggressive” physiotherapy the presence of a cyclops lesion should be considered. An MRI should be ordered to confirm the diagnosis and determine if surgical excision is in order. Though the median time for arthroscopic intervention is 16 weeks, cyclops lesions have been excised as long as 24 years from the initial trauma.
Though the mainstay of the literature presumptively attributes arthrofibrosis to be the source of the cyclops lesion, upon further review of the literature as well as histopathologic (microscopic) review of such lesions it becomes readily apparent that there may be more to the cause. The alternate hypothesis postulates that the cyclops lesion results from not only the natural fibroproliferative process but also largely from the drilling process of the tibial tunnel and bony fragments left after the drilling. Surgeons Jackson and Schaefer (1990) dramatically reduced the incidence of cyclops lesions in their operative ACL patients by following some basic tenets:
- a complete and meticulous debridement, or removal of all extra tissue and debris, as well as a clean out of the drilling debris at the joint side of the tibial tunnel
- specific avoidance of an anterior position of the tunnel, based on their postulated mechanism of cyclops genesis, in favour of a more anatomical location
Perhaps the most convincing evidence that the cyclops lesion is distinct from arthrofibrosis lies in its composition. Cyclops lesions were examined carefully and with the use of electron microscopy they were discovered to contain the following constituents: dense fibroconnective tissue rich in newly formed blood vessels, variable amounts of cartilage, bony tissue and occasionally some apparently dead bone. It is clear that the drilling debris from an ACL reconstruction plays a major role in the formation of these lesions. How else does one explain bony fragments and cartilaginous tissue within the Cyclops lesion?
Delince et al in 1998 during follow-up arthroscopy mooted multifactorial aspects playing a role in promoting a cyclops. These factors are various surgical factors such as inadequate removal of tissue especially bone fragment as well as of the ACL stump remnant, and malposition of the new graft. A graft that is not perfectly positioned can cause repeated microtrauma, and subsequent scar tissue formation, resulting in repeated graft impingement. This can be avoided intraoperatively by taking the time to enlarge the notch roof to eliminate any contact with the graft when the knee is fully extended.
How common is a Cyclops complication?
Some literature reviews cites rates of cyclops lesions from 1-9%, others up to 24%; neither of these is acceptable, as it seems that they are preventable, barring a small reasonable fraction of human error. The literature, seems to place the responsibility squarely on the surgeons’ shoulders. We as patients must advocate for themselves and ask their surgeons about their complication rates. Ask what the rates of revisiting the operating room are. Ask what the rates of revisiting the operating room for lysis of adhesions, excision of cyclops lesions, Behave in a way that is not rude but unapologetic for taking an active role in our medical care. The impact on our quality of lives, the need to change careers, is certainly worth the surgeon taking an extra 45 minutes in the operating room to make sure he or she has addressed all aspects of the surgery within his or her control to guarantee an exceptional outcome.
I was curious to know whether a particular graft was associated with a higher rate of Cyclops lesion as compared to others. Given the various types of ACL grafts we have to select from - patellar tendon grafts, hamstring grafts, cadaver grafts - in my literature review I sought to discern if one type of graft was more or less likely to precipitate a cyclops lesion. I could not find any literature to indicate that any one type of graft was immune. Cadaver grafts requiring less manipulation, I thought, may produce less cyclops lesions than patellar grafts, but that was not the case. If the precipitating factor in the triggering of a cyclops is indeed the drilling of the tibial tunnel with associated production of tiny bony fragments, it would stand to reason that no ACL graft is immune from this lesion. However, meticulous but time-consuming surgical technique using sequential drills of multiple diameters can be employed to decrease the production of bony fragments, and may save the patient from this inherent risk and an extended rehabilitation, only to lead to the inconvenience of a second trip to the operating room and another round of rehabilitation.
References
- Jackson DW, Schaefer Cyclops Syndrome: loss of extension following intra-articular cruciate ligament reconstruction. Arthroscopy 1990 6 (3) 171-178
- Delince P, Krallis P, Descamps PY, Different aspects of the cyclops lesion following anterior cruciate reconstruction: a multifactorial etiopathogenesis. Arthroscopy 1998 Nov-Dec; 14 (8) 869-876.
Extra reading
https://www.slideshare.net/drdsabat/complications-with-a-c-l-2014
